This privacy policy is to provide information to you, our patient, on how your personal information (which includes your health information) is collected and used within our practice, and the circumstances in which we may share it with third parties.
When you register as a patient of our practice, you provide consent for our GPs and practise staff to access and use your personal information so they can provide you with the best possible healthcare. Only staff who need to see your personal information will have access to it. If we need to use your information for anything else, we will seek additional consent from you to do this.
Our practise will need to collect your personal information to provide healthcare services to you. Our main purpose for collecting, using, holding and sharing your personal information is to manage your health. We also use it for directly related business activities, such as financial claims and payments, practise audits and accreditation, and business processes (eg staff training).
The information we will collect about you includes your:
You have the right to deal with us anonymously or under a pseudonym, unless it is impracticable for us to do so or unless we are required or authorised by law to only deal with identified individuals.
Our practise may collect your personal information in several different ways.
In some circumstances, personal information may also be collected from other sources. Often this is because it is not practical or reasonable to collect it from you directly. This may include information from:
We sometimes share your personal information:
Only people who need to access your information will be able to do so. Other than in the course of providing medical services or as otherwise described in this policy,
Our practice may use your personal information for marketing any of our goods or services directly to you without your express consent. If you do not consent, you may opt-out of direct marketing at any time by notifying our practice in writing. The practice may at its discretion, share personal information to 3rd parties only in the event where the practice deems it necessary to obtain better health outcomes for the patients.
Your personal information may be stored at our practice in various forms. Critical medical information such as paper records, electronic records, visual records (X-rays, CT scans, videos and photos), audio recordings. will only be stored digitally on our secure servers located within our practice.
Our practise stores all personal information securely. All electronic data are stored within protected information systems. Passwords are used by all members of staff. Dentist Near Me will try to protect your information; however, breaches from inside/outside are not the liability of Dentist Near Me. By accepting treatment of any of our practitioners for any reason, means you accept this risk and the potential of loss of privacy and information, as per the initial patient form.are personal information to 3rd parties only in the event where the practice deems it necessary to obtain better health outcomes for the patients.
You have the right to request access to, and correction of, your personal information.
Our practise acknowledges patients may request access to their medical records. We require you to put this request in writing and our practice will respond within a reasonable time. The process to hand over critical documents of a patient may take up to 30 days and may incur a fee as well. The standard minimum clinical fee for the transfer of records is $300 per record. This fee may increase depending on the difficulty of transfer and/ or type of documents (Workcover/ CTP or Lawyer documents).
Our practice will take reasonable steps to correct your personal information where the information is not accurate or up to date. From time to time, we will ask you to verify that your personal information held by our practice is correct and current. You may also request that we correct or update your information, and you should make such requests in writing to admin@dentistnearme.clinic.
We take complaints and concerns regarding privacy seriously. You should express any privacy concerns you may have in writing. We will then attempt to resolve it in accordance with our resolution procedure. Any such complaints can be made via our email (admin@dentistnearme.clinic) or through the phone (02) 9681 7886)
You may also contact the OAIC. Generally, the OAIC will require you to give them time to respond before they will investigate. For further information visit www.oaic.gov.au or call the OAIC on 1300 363 992.
The following statement is added onto the patient agreement, as an acknowledgement of the use of personal data:- “Personal information is collected in order to provide you with certain content, products and services and, unless you opt-out or unsubscribe, contact you in the future with information on products and services and to provide you with marketing materials via any medium including mail, telephone and commercial electronic messages (SMS (Short Message Service), MMS (Multimedia Message Service), IM (Instant Messaging) and email) or any other form of electronic, emerging, digital or conventional communications channel whether existing now or in the future.
We may also collect and use passively collected anonymous information or personal information from various third-party sources and may combine this anonymous information or personal information with other personal information collected from you, to provide better service to Website users, customise a Website based on your preferences, compile and analyse statistics and trends, and otherwise administer and improve its Websites for your use.”
Dentist Near Me will try to protect your information; however, breaches from inside/outside are not the liability of Dentist Near Me. By accepting the treatment of any of our practitioners for any reason, means you accept this risk and potential of loss of privacy and information, as per the initial patient form.
This policy will be reviewed on a biannual basis following any changes that may occur. Patients will be informed via email or SMS of any major changes within the practice.
The Privacy policy template for general practices is intended for use as a guide of a general nature only and may or may not be relevant to particular practices or circumstances. The Royal Australian College of General Practitioners (RACGP) has used its best endeavours to ensure the template is adapted for general practice to address current and anticipated future privacy requirements. Persons adopting or implementing its procedures or recommendations should exercise their own independent skill or judgement, or seek appropriate professional advice. While the template is directed to general practice, it does not ensure compliance with any privacy laws, and cannot of itself guarantee discharge of the duty of care owed to patients. Accordingly, the RACGP disclaims all liability (including negligence) to any users of the information contained in this template for any loss or damage (consequential or otherwise), cost or expense incurred or arising because of reliance on the template in any manner.
Dentist Near Me recognise the practice team requires access to email and the internet to assist in the efficient and safe delivery of healthcare services to our patients. Dentist Near Me support the right of staff to have access to limited personal use of the internet and email communications in the workplace using the devices and networks provided by the practice. By signing on as a new patient or using our services as a returning patient, you indemnify the practice from any data breaches via email or other communication forms. Email is not the most secure form of communication, however by not opting out our electronic communications on our patient forms or letting staff know you indemnify the practice of any breaches. You will be liable for any information that is requested to be sent via email. Results are sent via email as a form of communication. By using the services in Dentist Near Me, directly or indirectly, you indemnify the practice of any medical records breaches.
This policy sets out guidelines for acceptable use of the internet and email by the practice team, contractors and other staff of Dentist Near Me. Internet and email are provided primarily to assist the team carry out their duties of employment.
This internet and email policy apply to the practice team, contractors and other staff of Dentist Near Me who access the internet and email on practice owned devices, including, but not limited to desk phones, smartphones, tablets, laptops, desktop computers, iPads and other tablet devices to perform their work.
Use of the internet by the practice team, contractors and other staff is permitted and encouraged where this supports the goals and objectives of Dentist Near Me. Access to the internet is a privilege and the practice team, contractors and other staff must adhere to this policy.
Violation of these policies could result in
All employees are required to confirm they have understood and agree to abide by this email and internet policy verbally and at the start of their contract.
The practice team, contractors and other staff may use the internet and email access provided by Dentist Near Me for:
Limited personal use is permitted where it:
Examples of what could be considered reasonable personal use could be included in your policy and could include:
The practice team, contractors and other staff may not use internet or email access provided by Dentist Near Me to:
This policy will be reviewed regularly to ensure it reflects the current processes and procedures of Dentist Near Me and current legislation requirements.
Normal Times
Emails replies – 7 Days
Missed Call return – 1-2 Days
Fax responses – 1-2 Days
These timeframes can be exceeded during high volume periods, but staff will endeavour to get back to you as soon as possible.
Chaperone Policy
All clinical consultations, examinations and investigations are potentially distressing. Patients may find some examinations, collectively referred to as intimate examinations particularly intrusive. These can be examinations, investigations or photography involving the breasts, genitalia or anus (including vaginal & rectal examinations). Also, consultations involving dimmed lights, the need for patients to undress or for intensive periods of being touched, may make a patient feel vulnerable.
Summary
The relationship between a patient and their practitioner is based on trust. A practitioner may have no doubts about a patient they have known for a long time and feel it is not necessary to offer a formal chaperone. Similarly, studies have shown that many patients are not concerned whether a chaperone is present or not. However, this should not detract from the fact that it is good practice to offer all patients a chaperone if they feel one is required. Chaperone guidance is for the protection of both patients and staff and should always be followed. The key principles of communication and record-keeping will ensure that the practitioner/patient relationship is maintained and act as a safeguard against formal complaints, or in extreme cases, legal action.
Contained in this policy is practical advice to healthcare professionals working in a variety of locations on who, when and how to offer a chaperone and how to undertake record keeping.
The purpose of this document is to ensure that Dentist Near Me meets statutory requirements and minimises risks to patients, professional staff and the organisation, by ensuring that a systematic and planned approach for the provision of chaperones is in place.
A chaperone, in this clinical instance, is a third party present at a consultation that involves an intimate examination, as a safeguard for all parties and is a witness to continuing consent for the intervention.
Research shows that chaperones are most often required or requested where a male examiner is carrying out an intimate examination or procedure on a female patient. Complaints involving allegations of improper examination by a doctor are very rare, but where allegations of indecent assault during a clinical examination do occur almost all are against a male doctor and a small but significant minority of cases involve a male doctor and a male patient.
However, it is good practice for a health organisation to offer all patients a chaperone for any consultation, examination or procedure where the patient feels one is required. Staff should be aware that intimate examinations might cause anxiety for both male and female patients regardless of whether or not the examiner is of the same gender as the patient.
Staff should remember when acting as a chaperone they need to be in view and earshot of the patient and clinician. It may not be sufficient to be on the other side of the curtain although it will be considered to be the decision of the clinician.
There is no common definition of a chaperone and their role varies considerably depending on the needs of the patient, the healthcare professional, and the examination or procedure being carried out.
Broadly speaking their role can be considered in any of the following areas;
The role of a chaperone should be made clear to both the patient and the person who is undertaking the role.
Non-clinical chaperones should be told if assistance will be needed, such as assisting with undressing, helping on and off the examination bed. The chaperone can decline the role if not comfortable and an alternative is offered.
The designation of the chaperone will depend on the role expected of them and on the wishes of the patient.
If the chaperone is to ensure the appropriateness of clinical actions i.e. is expected to observe an intimate examination to ensure appropriateness or is to participate in the examination or procedure, then the chaperone must be clinical as non-clinical chaperones would not be able to comment on appropriateness.
If the chaperone is to have a passive role such as providing support to the patient during the procedure then a non-clinical chaperone would suffice.
Many patients feel reassured by the presence of a familiar person, such as a family member or close friend, and this request in almost all cases should be accepted. A situation where this may not be appropriate is where a child is asked to act as a chaperone for a parent undergoing an intimate examination. They may not necessarily be relied upon to act as a witness to the conduct or continuing consent of the procedure. However, if the child is providing comfort to the parent and will not be exposed to unpleasant experiences it may be acceptable for them to be present.
It is inappropriate to expect an informal chaperone to take an active part in the examination or to witness the procedure directly.
Clinicians should be wary at accepting the patients choice of chaperone, best practice would be to provide a chaperone from the surgery as well.
A formal chaperone implies a clinical health professional, such as a nurse, or a specifically trained non-clinical staff member, such as a receptionist. This individual will have a specific role to play in terms of the consultation and this role should be made clear to both the patient and the person undertaking the chaperone role. This may include assisting with undressing or assisting in the procedure being carried out. In these situations, staff should have had sufficient training to understand the role expected of them.
The patient should always have the opportunity to decline a particular person as a chaperone if that person is not acceptable to them for any reason. They should be made aware that in order to locate a replacement chaperone the procedure may be delayed or necessitate the appointment to be rescheduled. In all cases where the presence of a chaperone may intrude in a confiding clinician-patient relationship, their presence should be confined to the physical examination. One-to-one communication should take place separately.
Although it is good practice for all patients to be routinely offered a chaperone during any consultation or procedure, it does not mean that every consultation needs to be interrupted in order to ask if the patient wants a third party present. Ideally, the offer of a chaperone should be made prior to the actual consultation via prominently placed posters, practice leaflets and verbal information when booking appointments, although it is recognised that it is not always clear ahead of the consultation that an intimate examination or procedure is required.
A patient notification poster can be found in the waiting room, see Appendix A. Most patients will not take up the offer of a chaperone, especially where a relationship of trust has been built up or where the examiner is the same gender as them.
Patients decline the offer of a chaperone for a number of reasons; because they trust the clinician, therefore think one is unnecessary, require privacy or would find the situation too embarrassing with a third party present. For some patients, the level of embarrassment increases in proportion to the number of individuals present.
However, there are some cases where the clinician may feel unhappy to proceed unless a chaperone is present e.g. where there is a history of violent or unpredictable behaviour on behalf of the patient or their family member/friend.
If a chaperone is refused by the patient, a healthcare professional cannot usually insist that one is present, but where reasonably practicable in these situations it may be necessary to reschedule the appointment to enable the health professional to seek advice.
If the patient is offered and declines a chaperone, it is important that this is recorded.
If the patient has requested a chaperone the patient must be given the opportunity to reschedule their appointment within a reasonable timeframe.
If the seriousness of the condition would dictate that a delay is inappropriate then this should be explained to the patient and recorded in their notes. A decision to continue or otherwise should be jointly reached. In cases where the patient is not competent to make an informed decision then the healthcare professional must use their own clinical judgement, record their decision and be able to justify this course of action.
It is acceptable for a doctor (or another member of the health care team) to perform an intimate examination without a chaperone if the situation is life-threatening or speed is essential in the care or treatment of the patient. This should be recorded in the patients’ medical records.
It is assumed that in attending a consultation a patient is seeking treatment. However, before proceeding with an examination, healthcare professionals should always provide sufficient information for the individual to be able to make an informed decision to give consent. This may be by word or gesture, or some explicit indication that the patient understands the need for examination and agrees to it being carried out. Consent should always be appropriate to the treatment or investigation being carried out, and in some cases, written consent should be sought.
In the case of children, a chaperone would normally be a parent or carer or alternatively someone known and trusted or chosen by the child. For competent young adults, the guidance relating to adults is applicable.
Children and their parents or guardians must receive an appropriate explanation of the procedure in order to obtain their cooperation and understanding. If a minor presents in the absence of a parent or guardian the healthcare professional must ascertain if they are capable of understanding the need for examination. In these cases, it would be advisable for consent to be secured and a formal chaperone to be present for any intimate examinations.
Healthcare professionals should refer to the local Child Safeguarding Policies or contact the named GP or named Nurse.
The ethnic, religious and cultural background of some women can make intimate examinations particularly difficult. Some women have a strong cultural aversion to being touched by men other than their husbands, so in these cases, patients undergoing examinations should be allowed the opportunity to limit the degree of nudity by, for example, uncovering only that part of the anatomy that requires investigation or imaging.
It would be unwise to proceed with any examination if the healthcare professional is unsure that the patient understands due to a language barrier.
If an interpreter is available, they may be able to double as an informal chaperone. In life-saving situations, every effort should be made to communicate with the patient by whatever means available before proceeding with the examination.
For patients with learning difficulties or mental health problems that affect capacity, a familiar individual such as a family member or carer may be the best chaperone. A careful, simple and sensitive explanation of the technique is vital.
Where a healthcare professional is working in a situation away from other colleagues e.g. home visits, out-of-hours centres, the same principles for offering and use of chaperones should apply. In cases where a formal chaperone would be appropriate, i.e. intimate examinations, the healthcare professional would be advised to reschedule the examination to a more convenient location. However, in cases where this is not an option, for example, due to the urgency of the situation or because the practitioner is community-based, then procedures should be in place to ensure that communication and record-keeping are treated as paramount.
Healthcare Professionals should note that they are at an increased risk of their actions being misconstrued or misrepresented if they conduct intimate examinations where no other person is present.
Chaperones will stay within their described role and restrict their participation in the procedure as agreed in advance with the healthcare professional. On completion of the procedure, it may be appropriate for the chaperone to leave the patient to continue the consultation and discuss findings in private.
Details of the examination including presence/absence of chaperone and information given must be documented in the patient’s medical records. The following codes should be used: (these are also available through relevant templates.
Chaperone Offered
Chaperone Refused
Chaperone Present
The name of the chaperone should also be noted (including job role).
Consultation
This paper applies to all members of The Dentist Near Me
Current as of 3/12/2020
Name of social media officer: [Dr Saideepan Mohanadas | Practice Manager]
This policy provides guidance for members of the practice on using social media internally and externally. The policy helps identify and mitigate risks associated with social media use.
For the purposes of this policy, ‘social media is online social networks used to disseminate information through online interaction.
Regardless of whether social media is used for a business-related activity or for personal reasons, the following policy requirements apply to all GPs and practice staff of the practice. GPs and practice staff are legally responsible for their online activities, and if found to be in breach of this policy could result in:
The practice will appoint a staff member as a social media officer responsible for managing and monitoring the practice’s social media accounts. All posts on the practice’s social media website must be approved by this staff member. The practice reserves the right to remove any content at its own discretion.
When using the practice’s social media, practice staff will not:
– is unlawful, threatening, defamatory, pornographic, inflammatory, menacing or offensive
– infringes or breaches another person’s rights (including intellectual property rights) or privacy, or misuses the practice’s or another person’s confidential information (eg do not submit confidential information relating to our patients, personal information of staff, or information concerning the practice’s business operations that have not been made public)
– is materially damaging or could be materially damaging to the practice’s reputation or image, or another individual
– is in breach of any of the practice’s policies or procedures
– claim or imply that you are speaking on the practice’s behalf unless you are authorised to do so
– disclose any information that is confidential or proprietary to the practice, or to any third party that has disclosed information to the practice
The practice’s social media channels are part of our customer service and should be monitored and dealt with regularly. Response times for social media can be indefinite, however, we will attempt to reply within 30 days on a particular response. Complaints are taken seriously, and when brought to our attention are attempted to have immediate action. All Platforms are updated ASAP but within reason.
The practise complies with AHPRA national law and takes reasonable steps to remove testimonials that advertise their health services (which may include comments about the practitioners themselves). The practice is not responsible for removing (or trying to have removed) unsolicited testimonials published on a third-party website or in social media accounts over which they do not have control.
Staff are free to personally engage in social media outside of work hours, as long as their actions do not have the potential to bring the practice into disrepute. Employees may not represent personal views expressed as those of this practice.
Any social media posts by staff on their personal social media platforms must not reveal confidential information about the practice or a person who uses the practice (eg staff should not post information relating to patients or other staff, or information concerning the practice’s business operations that have not been made public).
Staff should respect copyright, privacy, fair use, financial disclosure and other applicable laws when publishing on social media platforms.
Dentist Near Me require staff to include a disclaimer if they identify themselves as a practice employee on any social media platforms, when in discussion about the medical centre. ‘The views expressed in this post are mine and do not reflect the views of the practice/business/committees/boards of which I am a member’.
All social media activities must be in line with this policy.
The policy will be reviewed regularly to ensure it is up to date with changes in social media or relevant legislation. We update this document which staff needs to check on a regular basis (every 3 months at a minimum), when changes are made.
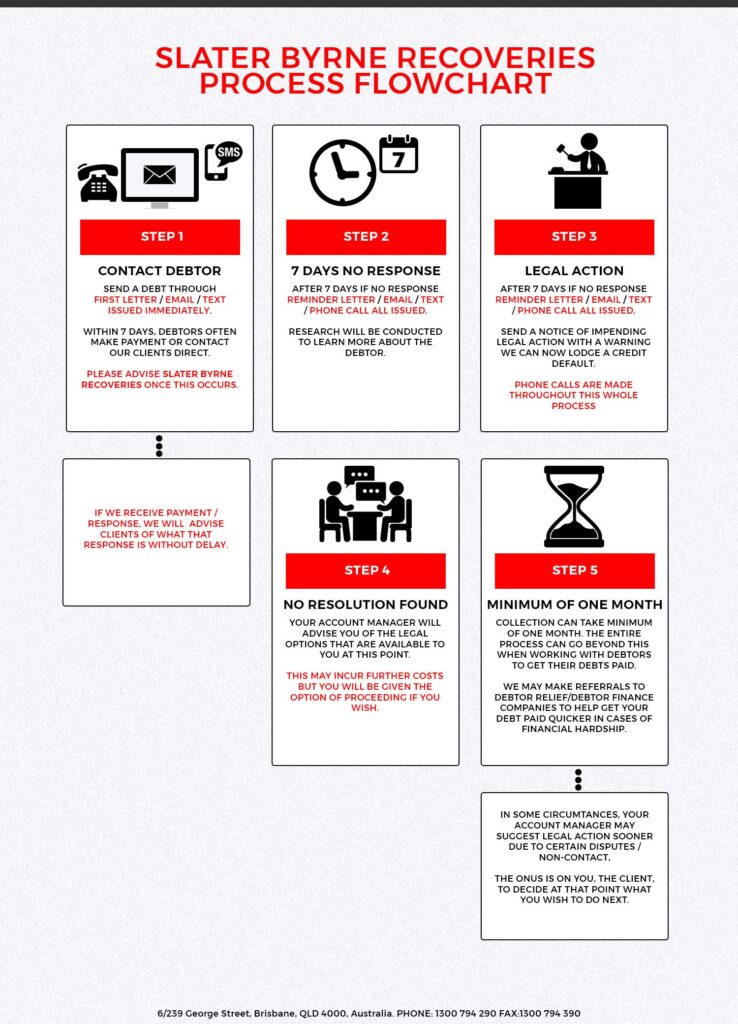
All Collections are outsourced to Slater and Byrne, and their collection policies are outlined below. By Signing the new patient form you agreed to the conditions below. All collection fees and legal fees are payable by the debtor.
This system is ideal for managing the collection of smaller debts (of usually under $1,000.00), where legal action may not be considered a viable alternative.
It is a low cost and effective way of communicating with your slow paying debtors and prompting them to bring their accounts up to date.
You are responsbile for all payments in full. Any debts outstanding will have 10% interest per month outstanding compunded daily. Any debt collection fees and legal fees will also be added to the amount owed.
Statements and Tax Invoices are forwarded to you via email at each end of month.
Each statement will either itemise the direct deposit details of funds remitted from our Trust account to your nominated account, after deduction of any costs or commission incurred and not previously reimbursed by you, or alternatively may request payment of disbursements outlaid on your behalf.
All costs and commission (other than court filing fees and exempt government fees) are subject to GST.
All debit Statements are payable within 14 days of issue to you.
It is at the discretion of Dentist Near Me to pursue debts owed. The third party company that debts are outsourced to may change, and may not be updated in this policy. The policy outlined above may not be current. By signing the patient declaration form, you agree to indemnify us about any lack update in this document or an inaccuracies in the information above.
Current as of: 19/10/2020
This policy provides information on e-waste management within our practice.
Dentist Near Me is committed to addressing the following issues in relation to e-waste in the practice:
We will inform and motivate all of our staff and encourage them to play an active role in Dentist Near Me commitment to its e-waste disposal/environmental policy.
Prior to discarding electronic equipment, we will ensure all records stored on this equipment are removed and destroyed in such a way as to render them unreadable and leave them in a form which they cannot be reconstructed in whole or in part. We will use Mednology to complete this process.
We will donate any redundant electronic equipment to Mednolog. If electronic equipment is beyond repair, we will utilise the services of Mednology to recycle this equipment. We will favour suppliers and contractors that are reputable and adopt best environmental practices.
We will continue to promote, develop and implement waste prevention, reduction, reuse and recycling on-site in a systematic and cost effective manner. We will use appropriately regulated waste management contractors to ensure safe management of hazardous and non-hazardous waste sent off-site in accordance with best environmental practice.
This policy informs patients about the practice’s standards regarding the prescription of drugs of dependence.
Many of our patients require strong, potentially addictive medication to help manage their condition(s). Of concern are ‘drugs of dependence’ (eg opioid medications and benzodiazepines), particularly when these are prescribed on an ongoing basis. Due to increasing reports of abuse of prescription drugs and patient behavioural problems, Dentist Near Me has established a policy to ensure adequate treatment of your condition, while reducing the risk of problems with drug prescriptions.
The major points are described below.
If you are a new patient to the practice:
It may take time to get accurate medical information about your condition. Until such information is available, your GP may choose not to prescribe any medication. It is our policy that GPs do not prescribe drugs of dependence until they have a full clinical picture.
Your GP may decide not to continue prescribing an opioid medication previously prescribed for you. It may be determined that such a medication is not suitable. It is our policy that GPs do not prescribe drugs of dependence if they feel that previous prescriptions were inappropriate.
Your GP will evaluate your condition and only prescribe an opioid of the strength necessary for you. This may be different than what another doctor may have given you in the past.
General practice standards:
If the decision to prescribe is taken after a shared discussion of goals, plans, risks and benefits, you may be required to confirm your consent in writing.
You may be asked to sign a contract that will detail our practice’s expectations when prescribing drugs of dependence. This contract details your responsibilities as a patient taking a drug of dependence; any prescriptions issues; advice on taking your medications; how we will monitor your care; and the standards of behaviour that are expected.
Patients may need to acknowledge that their care requirements may be complex, and that referral for ongoing care for all or part of your healthcare may be required. It is our practice policy that patient care is matched with the level of complexity.
Patients are reminded that we have a zero tolerance on issues relating to staff abuse. Any threats to staff will result in transfer of your care.
Introduction
Why this is important
The ideal patient-practitioner partnership is a collaboration based on mutual respect and mutual responsibility for the patient’s health. The clinician’s duty of care includes clearly explaining the benefits and potential harm of specific medical treatments and the consequences of not following a recommended management plan.
Understanding what respectful and culturally appropriate care is
Respectful and culturally appropriate care is based on cultural awareness and sensitivity, which begins with learning about other cultures and cultural beliefs. Cultural awareness is defined by the Centre for Cultural Diversity in Ageing as:
An understanding of how a person’s culture may inform their values, behaviours, beliefs and basic assumptions … [It] recognises that we are all shaped by our cultural background, which influences how we interpret the world around us, perceive ourselves and relate to other people.
Cultural safety, defined in Binan Goonj: Bridging cultures in Aboriginal health as ‘an outcome of health practice and education that enables safe service to be defined by those who receive the service’,9 is the consequence of behavioural changes that come about after there is cultural awareness. Culturally safe policies aim to create an environment that is ‘safe for people: where there is no assault, challenge or denial of their identity, of who they are and what they need, where there is ‘shared respect, shared meaning, shared knowledge and experience, of learning, living and working together with dignity and truly listening.
Patient’s rights
Patients have the right to respectful care that considers their religion and cultural beliefs, displays an acceptance of diversity and promotes their dignity, privacy and safety. Respect for a patient extends to recording, storing, using and disclosing health and other information about them. You need to understand the demographics and cultural backgrounds of your patient population so that you can provide the most appropriate care. When clinical team members ask patients about their cultural identity and beliefs in order to update the patient’s details, it is beneficial to explain that this helps the practice to provide culturally sensitive care. All members of the practice team need to have interpersonal skills that allow them to successfully interact with patients and colleagues. 26 RACGP Standards for general practices, 5th edition Be mindful that when dealing with patients, the practice team must also comply with Commonwealth and any relevant state or territory anti-discrimination laws.
Rights to refuse treatment and obtain second opinions
Patients with decision-making capacity have the right to refuse a recommended treatment, advice or procedure and to seek clinical opinions from other healthcare providers.
Patients’ responsibility
Patients have a responsibility to be respectful and considerate towards their practitioners and other practice team members.
Ethical dilemmas
Practitioners often need to manage ethical issues and dilemmas in many different primary healthcare situations. These can range from bioethical dilemmas (including end-of-life care and pregnancy termination) to receiving gifts from patients.
Respectful and culturally appropriate care
You could consider factors that may affect the provision of respectful and culturally appropriate care, including
Practitioners have a professional obligation to take reasonable care when taking a history from a patient and developing management plans. They must also ensure there is clear and effective communication in the patient-practitioner relationship so that they can effectively manage the patient’s healthcare. The patient needs to understand the discussion that takes place and needs to understand the proposed management and treatment. This may require the use of translating services. If a carer has an ongoing role in the day-to-day care of a patient, it is generally advisable to include the carer in the patient-practitioner relationship with the permission of the patient (if the patient is able to give such consent). Patients will also feel respected if the reception staff are positive, friendly, attentive, empathetic and helpful.
Managing health inequalities
Understanding local health inequalities allows your practice to identify opportunities to provide tailored healthcare to specific patients or patient groups. To develop an understanding of your practice population, you can either analyse practice data or use publicly available information.
Refusal of treatment or advice
Patients may refuse a practitioner’s recommended course of action, including advice, procedure, treatment or referral to other care providers.
When this happens, the practice may manage any associated risks by recording in the patient’s health record:
Second opinions
If the practitioner is aware that the patient wishes to seek another clinical opinion they could offer to provide a referral to the provider who is to give that opinion. Document in the patient’s health record:
You can also encourage patients to notify their practitioner when they decide to follow another healthcare provider’s advice so that the practitioner can discuss any potential risks of this decision.
Deciding to no longer treat a patient
If a practitioner no longer considers that it is appropriate to treat a particular patient, the steps taken to help the patient receive alternative ongoing care need to be recorded in the patient’s health record.
Dealing with distressed patients
You may develop a plan to help patients and other relevant people who are distressed and to ensure that they are treated respectfully. For example, you can provide a private area (such as an unused room or the staff room) where the person can wait before seeing a practitioner.
Ethical dilemmas
Examples of situations that might create ethical dilemmas in a practice include
We discuss these items via a safety and learning activities form. We discuss this as a team during our fortnightly team meetings and if required medical indemnity insurance.
Staff requirements
Follow cultural safety policy for the practice team and patients so that your practice team knows they are required to provide care that is respectful of a person’s culture and beliefs, and that is free from discrimination
Understand patients’ rights and responsibilities
No discrimination with staff, patients or contractors.
Target Audience
This paper applies to all members of The Dentist Near Me (patients and staff)